

Histopathologic abnormalities in PMD resemble keratoconus. A recent case showed that PMD was coexistent with corneal plana in an individual with a KERA mutation, thus, potentially implicating KERA in the development of PMD.
PMD has no sex or racial predilection, and does not appear to be hereditary, but moderate to high astigmatism has been noted in families with affected patients. PMD typically presents in the second to fifth decade of life. It has not been elucidated whether keratoconus, keratoglobus, and PMD are different diseases or phenotypic variations of the same disease.
#Pellucid marginal degeneration icd 9 series#
In series performed in Japan, 17 of 27 cases of unilateral PMD revealed keratoconus or suspected keratoconus in the fellow eye. Ten percent of PMD cases are associated with keratoconus and 13% are associated with keratoglobus. Keratoconus, keratoglobus, and PMD are postulated to be related because these conditions coexist in families. Some people postulate, however, that this prevalence might be underestimated as the condition is often misdiagnosed as keratoconus. PMD, while rare, is the second most common noninflammatory corneal thinning disorder after keratoconus. Also, patients who undergo refractive surgery with PMD can have deleterious results, so it is important to consider prior to refractive surgery. It is important to recognize as it can cause severe deterioration in visual function.

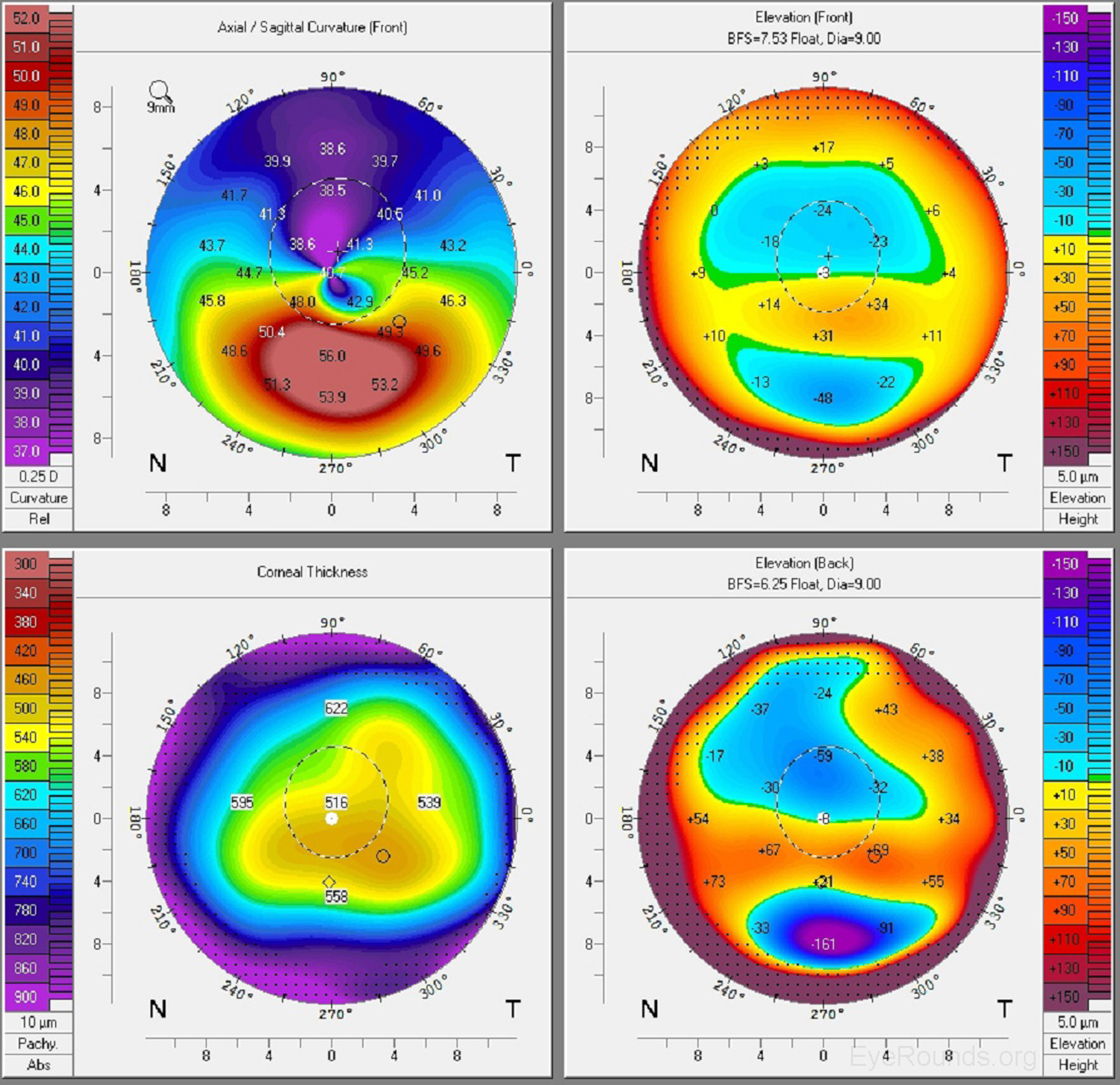
PMD is disease of peripheral corneal thinning that is slowly progressive over many years. There is no associated inflammation and the central cornea is of normal thickness. PMD is uncommon and is characterized by a crescent-shaped band of inferior corneal thinning approaching 20% of normal thickness that is 1 to 2 mm in height, 6 to 8 mm in horizontal extent, and 1 to 2 mm from the limbus.


 0 kommentar(er)
0 kommentar(er)
